Connect With Us
Blogs

Podiatrists Can Manage Cracked Heels

Cracked heels are a common foot condition characterized by fissures or splits in the skin, typically on the heels. They develop due to a combination of factors including dryness, pressure, and callus formation. Common causes include prolonged standing, wearing open-back shoes, obesity, and dry skin conditions like eczema or psoriasis. Besides being unattractive, cracked heels can become painful, especially if deep fissures form, leading to bleeding or infection risk. Calluses often accompany cracked heels, exacerbating discomfort. If left untreated, severe cases may lead to infections or difficulty while walking. Podiatrists are trained to diagnose and treat cracked heels effectively. They can remove thickened skin and calluses, offer advice on moisturizing and proper footwear, and address underlying conditions contributing to the problem. Additionally, they may recommend orthotic inserts to relieve pressure on the heels and prevent further cracking. If you have cracked heels that are painful or unsightly, it is suggested that you schedule an appointment with a podiatrist who can offer relief remedies.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Achilles Tendon Pain

If you are experiencing pain in the back of your heel, you may have injured your Achilles tendon. This tendon, named after the legendary Greek warrior Achilles, connects the calf muscles to the heel bone. Achilles tendon injuries are common among athletes, particularly in sports like basketball and soccer. Symptoms include pain in the back of the heel or up the back of the leg, ranging from mild to severe. These injuries can occur in different places along the tendon, with the most serious being Achilles tendinopathy, which involves chronic inflammation and fluid buildup. Treatment typically involves rest, gentle stretching, and strengthening exercises. Prevention strategies include paying attention to foot mechanics, adjusting running stride, and building flexibility and strength in the lower legs through targeted exercises. If you are experiencing pain in your Achilles tendon area, it is suggested that you make an appointment with a podiatrist for an evaluation and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Gentle Stretches for Sever's Disease
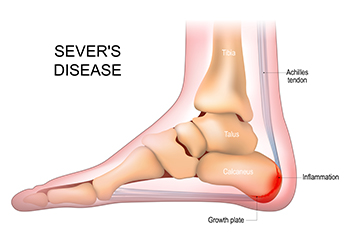
Sever's disease, a common heel condition among active children, can cause discomfort, but incorporating gentle stretches into daily routines can offer relief. Targeting the calf muscles, a simple standing calf stretch involves placing the affected foot behind the other, pressing the heel into the ground. The soleus stretch, achieved by bending the knee while keeping the heel on the floor, targets the deeper calf muscles. Additionally, the seated hamstring stretch aids in maintaining flexibility in the lower leg. Gentle Achilles stretches, with a focus on controlled movements, can also contribute to easing the tension associated with Sever's disease. Incorporating these stretches into daily activities promotes flexibility and aids in managing discomfort. To prevent exacerbating symptoms, it is important to perform these exercises consistently and avoid overexertion. If your active child has heel pain, it is strongly suggested that you confer with a podiatrist who can diagnose and offer additional relief options.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
Let the Expert Treat Your Ingrown Toenails
Neuropathy and Burning Feet

Experiencing a persistent burning sensation in your feet may indicate neuropathy has developed. The sensation of burning feet often results from nerve damage and is a common cause of this type of discomfort. While diabetes related neuropathy can be easily diagnosed, sudden or rapidly worsening unexplained burning sensations may necessitate comprehensive testing. Diagnostic measures include electromyography, or EMG, to assess muscle function, and nerve conduction studies to evaluate impulse transmission. In rare cases, a nerve biopsy may be conducted for microscopic examination. Laboratory tests such as blood, urine, or spinal fluid analysis may also help to identify underlying causes, such as vitamin E deficiency or uremia. Tailoring treatment for burning feet to the underlying cause is essential. For diabetic patients, treatment involves blood sugar control, insulin, diet changes, and oral medication. Alcohol induced neuropathy requires abstinence for nerve recovery. Chronic kidney failure may necessitate dialysis, and hypothyroidism calls for synthetic thyroid hormones. If you suspect neuropathy may be the cause of burning feet, it is suggested that you schedule an appointment with a podiatrist who is trained to manage foot conditions that stem from neuropathy.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Types of Ankle Fractures

Ankle fractures are common in injuries, making up approximately 10 percent of all fractures in trauma cases. They usually occur more in young men and older women. When there is a bigger accident with multiple injuries, ankle problems can greatly interfere with movement. There are different ways to classify ankle fractures. One way was introduced by Percival Pott, who looked at how many parts of the ankle bones got broken. There are two other systems called Lauge-Hansen and Danis-Weber that also offer ways to think about how the injury happened and how stable the break is. Each system offers good information. When doctors look at X-rays of ankle fractures, they have a certain way to approach repair. Fixing a displaced ankle fracture and making it line up right usually gives good results. But sometimes, even with the bones in the right place, the ankle can still have problems later because the cartilage is involved. About 15 percent of people may have arthritis in their ankle after this kind of fracture. If you have sustained an ankle fracture, it is suggested that you schedule an appointment with a podiatrist to have appropriate tests taken, a diagnosis made, and appropriate treatment offered.
Broken ankles need immediate treatment. If you are seeking treatment, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.