Connect With Us
Blogs

How Is Gout Diagnosed?

Gout, a form of inflammatory arthritis, emerges from the crystallization of uric acid within joints, particularly in the lower extremities. Elevated levels of uric acid, a natural by-product of purine metabolism, lead to the formation of needle-like crystals that trigger intense pain and inflammation, typically affecting the big toe. The primary contributors to gout include a diet rich in purine-containing foods, impaired kidney function hindering uric acid elimination, and a genetic predisposition. Diagnosing gout involves a comprehensive examination, including a detailed medical history, assessment of symptoms, and often the identification of characteristic crystal deposits through joint fluid analysis. The diagnostic process aims to differentiate gout from other joint disorders, ensuring accurate and timely intervention. Recognizing the causative factors and employing precise diagnostic measures are pivotal steps in comprehending and effectively managing gout, a condition that can significantly impact an individual's quality of life. If you have pain in your big toe, it is suggested that you consult a podiatrist who can accurately diagnose and treat gout.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Gout
Gout is a form of arthritis that is caused by a buildup of uric acid crystals in the joints. This considered to be one of the most frequently recorded medical illnesses throughout history. Gout occurrences in the US have risen within the past twenty years and the condition now affects 8.3 million people which is 4% of all Americans. Researchers have found that gout affects men more than women and African-American men more than white men.
Symptoms of gout are warmth, swelling, discoloration, and tenderness in the affected joint area. The small joint on the big toe is the most common place for a gout attack to occur.
People who are obese, gain weight excessively, drink alcohol heavily, have high blood pressure, or have abnormal kidney function are more likely to develop gout. Furthermore, certain drugs and diseases are likely to increase levels of uric acid in the joints which eventually leads to gout. You are also more likely to develop gout if you eat a lot of meat and fish.
Many who experience gout attacks will experience repeated attacks over the years. Some people who have gout symptoms, may never have them again, but others may experience them several times a year. If you have gout symptoms throughout the year, you may have recurrent gout. Those who have gout should also be careful about their urate crystals collecting in their urinary tract, because this may lead to kidney stones.
Diagnosis for gout is done by checking the level of uric acid in the joints and blood. Your podiatrist may also prescribe medicine to reduce uric acid buildup in the blood, which will help prevent any gout attacks.
To treat gout, your podiatrist may also prescribe you Anti-inflammatory medication (NSAIDs) which will relieve the pain and swelling of a gout episode and it can also shorten a gout attack. Maintaining a healthy diet is also a proven method to prevent gout attacks.
Stress Fractures and Risk Factors
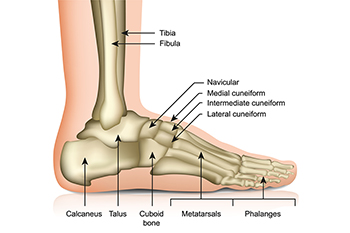
Foot stress fractures are tiny cracks in the bones resulting from repetitive force or overuse. These fractures, often seen in the metatarsal bones of the foot, can be subtle but carry the potential for significant discomfort and impairment if not addressed promptly. Risk factors contributing to the development of foot stress fractures are multifaceted. High-impact activities, such as running or jumping, increase the repetitive stress on the bones, making athletes more susceptible. Inadequate footwear or sudden increases in activity levels can also elevate the risk. Conditions like osteoporosis, which weakens bone density, may exacerbate the susceptibility to stress fractures. Nutritional deficiencies, particularly in calcium and vitamin D, compromise bone strength and resilience. Understanding both the definition and the spectrum of risk factors associated with foot stress fractures enables individuals to make informed choices about their physical activities, footwear, and overall bone health. If you have endured a stress fracture, it is suggested that you visit a podiatrist who can effectively treat this condition.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Insights Into Plantar Fasciitis

Plantar fasciitis, a prevalent foot ailment, reveals itself as a condition marked by inflammation of the plantar fascia, a band of tissue connecting the heel bone to the toes. Characterized by stabbing pain, particularly during the initial steps after awakening or prolonged periods of inactivity, plantar fasciitis often affects the heel and sole. The condition typically results from overuse, where repetitive stress on the plantar fascia leads to microtears and inflammation. While commonly associated with athletes, plantar fasciitis can affect individuals from various walks of life, particularly those with jobs that require prolonged standing. Having tight calf muscles or flat feet and wearing inadequate footwear may contribute to increased vulnerability. Recognizing plantar fasciitis's early signs, such as localized pain and stiffness, enables timely intervention. If you have heel pain, it may be indicative of plantar fasciitis. If this applies to you, it is strongly suggested that you visit a podiatrist who can diagnose and treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
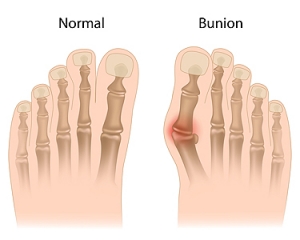
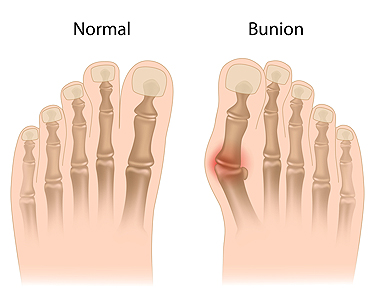
Causes and Treatment for Bunions
Bunions are painful bumps at the base of the big toe, primarily the result of hallux valgus, where the big toe deviates outward and tilts toward the second toe. Contributing factors for the formation of bunions include foot pronation, wearing tight shoes, injuries, osteoarthritis, and heredity. Bunions can cause pain, especially in narrow shoes, and may enlarge over time. Painful swelling caused by inflamed bursa under the toe often accompanies bunions and limits joint motion. Diagnosing bunions relies on symptoms and physical exams, such as X-rays, while joint fluid analysis rules out infectious arthritis or gout. Treatment options depend on the severity of the bunion. A podiatrist can guide you toward non-invasive treatment solutions, including orthotics, nonsteroidal anti-inflammatory medication, and corticosteroid injections to manage pain and inflammation. In severe cases, or when more conservative measures fail, surgical bunionectomy becomes an option. This procedure corrects joint alignment and removes the bunion. To determine the best treatment plan for your specific needs and taking into account the severity of your bunion, it is suggested that you make an appointment with a podiatrist.
If you are suffering from bunions, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Broken Toes Can Result in Complications

People can drop a heavy object on their foot, and may wonder if it is a temporary pain or something more serious like a broken toe. Broken toes are often the result of such accidents as having a heavy object drop on the foot, jamming it into a piece of furniture, or from missing a step. They can also occur due to an aggravated stress fracture, abnormal foot structure, or conditions such as osteoporosis. When a toe breaks, it causes severe pain, swelling, and bruising. Walking becomes difficult, but it is important to note that the ability to walk on a broken toe does not rule out a fracture. Diagnosis typically involves a visual examination and may require X-rays to be taken. Treatment options range from rest and elevation for minor fractures to splinting or buddy taping for more severe cases. In rare instances, surgery may be necessary to ensure proper healing. Complications such as toenail trauma, chronic pain, stiffness, and deformity can arise if a broken toe is not treated correctly. If you suspect you have broken your toe, it is suggested that you schedule an appointment with a podiatrist for a timely and effective recovery.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.