Connect With Us
Blog

Insights Into Plantar Fasciitis

Plantar fasciitis, a prevalent foot ailment, reveals itself as a condition marked by inflammation of the plantar fascia, a band of tissue connecting the heel bone to the toes. Characterized by stabbing pain, particularly during the initial steps after awakening or prolonged periods of inactivity, plantar fasciitis often affects the heel and sole. The condition typically results from overuse, where repetitive stress on the plantar fascia leads to microtears and inflammation. While commonly associated with athletes, plantar fasciitis can affect individuals from various walks of life, particularly those with jobs that require prolonged standing. Having tight calf muscles or flat feet and wearing inadequate footwear may contribute to increased vulnerability. Recognizing plantar fasciitis's early signs, such as localized pain and stiffness, enables timely intervention. If you have heel pain, it may be indicative of plantar fasciitis. If this applies to you, it is strongly suggested that you visit a podiatrist who can diagnose and treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Causes and Treatment for Bunions
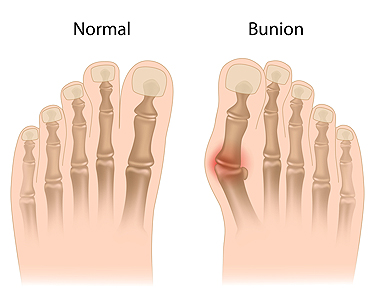
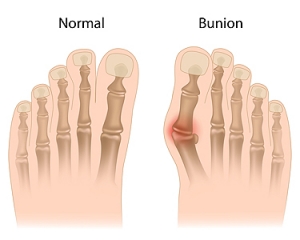
Bunions are painful bumps at the base of the big toe, primarily the result of hallux valgus, where the big toe deviates outward and tilts toward the second toe. Contributing factors for the formation of bunions include foot pronation, wearing tight shoes, injuries, osteoarthritis, and heredity. Bunions can cause pain, especially in narrow shoes, and may enlarge over time. Painful swelling caused by inflamed bursa under the toe often accompanies bunions and limits joint motion. Diagnosing bunions relies on symptoms and physical exams, such as X-rays, while joint fluid analysis rules out infectious arthritis or gout. Treatment options depend on the severity of the bunion. A podiatrist can guide you toward non-invasive treatment solutions, including orthotics, nonsteroidal anti-inflammatory medication, and corticosteroid injections to manage pain and inflammation. In severe cases, or when more conservative measures fail, surgical bunionectomy becomes an option. This procedure corrects joint alignment and removes the bunion. To determine the best treatment plan for your specific needs and taking into account the severity of your bunion, it is suggested that you make an appointment with a podiatrist.
If you are suffering from bunions, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Broken Toes Can Result in Complications

People can drop a heavy object on their foot, and may wonder if it is a temporary pain or something more serious like a broken toe. Broken toes are often the result of such accidents as having a heavy object drop on the foot, jamming it into a piece of furniture, or from missing a step. They can also occur due to an aggravated stress fracture, abnormal foot structure, or conditions such as osteoporosis. When a toe breaks, it causes severe pain, swelling, and bruising. Walking becomes difficult, but it is important to note that the ability to walk on a broken toe does not rule out a fracture. Diagnosis typically involves a visual examination and may require X-rays to be taken. Treatment options range from rest and elevation for minor fractures to splinting or buddy taping for more severe cases. In rare instances, surgery may be necessary to ensure proper healing. Complications such as toenail trauma, chronic pain, stiffness, and deformity can arise if a broken toe is not treated correctly. If you suspect you have broken your toe, it is suggested that you schedule an appointment with a podiatrist for a timely and effective recovery.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Complex Regional Pain Syndrome in the Foot

Complex Regional Pain Syndrome, or CRPS, in the foot is a condition where foot pain becomes intense and persistent, often after an injury or surgery. It can make your foot extremely sensitive to touch, and even the slightest contact may cause severe pain. Additionally, your foot may change in appearance, becoming swollen or discolored. You may find it challenging to move your foot and use your muscles properly. CRPS in the foot can be diagnosed through a physical examination and tests such as X-rays or nerve tests. While it is a complex condition, there are treatments available. If you are experiencing unusual or severe foot pain, it is strongly suggested that you schedule an appointment with a podiatrist to create a personalized plan to regain comfort and function in your foot, which may involve exercises and pain management techniques.
Some foot conditions may require additional professional care. If you have any concerns, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
Finding Shoes That Fit Well

Choosing shoes that fit correctly is a nuanced process that directly impacts comfort and foot health. Start by knowing your foot size, which can change over time and may differ between brands. It is beneficial to prioritize comfort over style, as shoes that feel good are more likely to provide adequate support. Ensure there is enough room for your toes to move and avoid tightness in the toe box, which can lead to discomfort and deformities over time. The arch support should match the natural curve of your foot. It's important to pay attention to the width, as shoes that are too narrow or too wide can cause friction and pressure points. Walk around in the shoes before purchasing to assess overall comfort and ensure a snug fit. Different shoe types may require slight adjustments in sizing. If you would like more information about how to find shoes that fit right for your feet, it is suggested that you confer with a podiatrist.
Getting the right shoe size is an important part of proper foot health. Seek the assistance of Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will provide the care you need to keep you pain-free and on your feet.
Getting the Right Shoe Size
There are many people who wear shoes that are the incorrect size, negatively affecting their feet and posture. Selecting the right shoes is not a difficult process, so long as you keep several things in mind when it comes to choosing the right pair.
- When visiting the shoe store, use the tools available to measure your foot.
- Be sure there is ‘wiggle room’. There should be about an inch between your toes and the tip of your shoes.
- Do not always assume you are the same size, as manufacturers run differently.
- Purchase shoes later in the day, as your feet swell as the day progresses.
- If a shoe is not comfortable, it is not suitable. Most shoes can’t be ‘broken in’, and comfort should be the ultimate goal when it comes to choosing the right pair of shoes
As our feet hold our body weight and keep us moving, it is important to treat them right. Picking the right pair of shoes can provide your feet comfort and mobility without pain.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.