Connect With Us
Blog

Divers Can Develop Fin Foot

Divers should be wary of a condition known as fin foot, causing swollen and tender feet after diving, often exacerbated in cold or rough waters. The discomfort of fin foot stems from reduced blood flow to the feet, due to factors like improper fin techniques or ill-fitting gear. Symptoms of fin foot can include swelling, redness, bruising to the toes, and pain while walking. Experts suggest that a diver experiencing these symptoms immediately cease diving, elevate their feet, and apply a warm compress for relief. Symptoms that persist beyond 48 hours warrant consultation with a podiatrist. Collaborating with a podiatrist ensures proper gear fit, including booties and fin straps. Adjustments, such as using larger booties or spring straps, can reduce the risk of recurrence. While edema in fin foot does not necessarily signify decompression sickness, divers are wise to remain vigilant to its effects. If you are experiencing post-dive foot problems, it is suggested that you schedule an appointment with a podiatrist.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
Care and Treatment of Bunions
 Bunions are a common foot problem, particularly prevalent among women. These bony bumps form on the joint at the base of the big toe, causing the big toe to lean towards the others. They develop due to genetic factors, foot structure, and wearing tight or ill-fitting shoes. Conditions such as arthritis can also contribute to bunion formation. Bunions can cause significant discomfort, including pain, swelling, and redness surrounding the affected joint. The skin over the bunion may become thickened and sore, making it difficult to walk or wear certain shoes, and often leading to embarrassment when wearing open-toe shoes. Caring for bunions involves wearing comfortable, well-fitting shoes with ample toe space, and avoiding high heels. Using padded shoe inserts or bunion pads can alleviate pressure and reduce pain. Taking pain relievers can help manage symptoms. In severe cases, bunions can lead to arthritis, and surgery may be necessary to correct the deformity. For persistent pain or severe bunions, it is suggested that you visit a podiatrist for professional treatment options.
Bunions are a common foot problem, particularly prevalent among women. These bony bumps form on the joint at the base of the big toe, causing the big toe to lean towards the others. They develop due to genetic factors, foot structure, and wearing tight or ill-fitting shoes. Conditions such as arthritis can also contribute to bunion formation. Bunions can cause significant discomfort, including pain, swelling, and redness surrounding the affected joint. The skin over the bunion may become thickened and sore, making it difficult to walk or wear certain shoes, and often leading to embarrassment when wearing open-toe shoes. Caring for bunions involves wearing comfortable, well-fitting shoes with ample toe space, and avoiding high heels. Using padded shoe inserts or bunion pads can alleviate pressure and reduce pain. Taking pain relievers can help manage symptoms. In severe cases, bunions can lead to arthritis, and surgery may be necessary to correct the deformity. For persistent pain or severe bunions, it is suggested that you visit a podiatrist for professional treatment options.
If you are suffering from bunion pain, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Definition and Symptoms of Plantar Warts

Plantar warts are common viral skin infections that occur on the soles of the feet, caused by the human papillomavirus, abbreviated HPV. These warts often appear as small, rough growths that can be painful when pressure is applied, such as during walking or standing. Characteristically, plantar warts may have tiny black dots on their surface, which are actually small, clotted blood vessels. The skin around the wart may become thickened or callused due to the constant friction and pressure. In some cases, plantar warts can cluster together to form mosaic warts, which can be particularly difficult to treat. Symptoms can include tenderness and discomfort, particularly when the wart is located on a weight-bearing area of the foot. The majority of people experience pain while walking with plantar warts. If this applies to you, it is suggested that you consult a podiatrist who can offer you effective relief and treatment solutions.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
What Can Cause Cracked Heels?
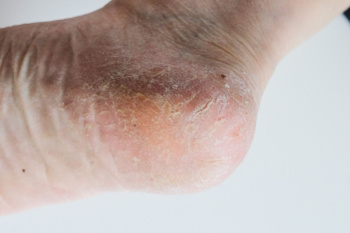
Cracked heels, a common foot ailment, can be caused by various factors. Vitamin deficiencies, particularly in vitamins A, C, and E, can lead to dry, flaky skin, making heels more prone to cracking. Excess weight gain places added pressure on the heels, leading to calluses and fissures. Wearing ill-fitting or open-back shoes exposes the heels to friction and pressure, exacerbating the problem. Additionally, genetics may also play a role, as some individuals naturally have drier skin or a predisposition to foot conditions. Unhygienic conditions, such as standing for long periods in damp environments or neglecting proper foot care, can contribute to cracked heels. Cracked heels can cause significant pain and discomfort. If this applies to you, it is strongly suggested that you confer with a podiatrist who can prescribe medication for effective relief.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Symptoms of a Jones Fractures

Among the array of foot injuries, a Jones fracture demands rigorous attention. A Jones fracture, or avulsion fracture, occurs when a tendon or ligament forcefully pulls a small piece of bone away from the main bone. In the case of a Jones fracture, this typically occurs in the fifth metatarsal bone, which connects the pinky toe to the rest of the foot. This type of injury is often the result of a significant and direct impact, causing intense pain. Pain at the base of the foot is a primary symptom and should never be ignored, even if other symptoms are absent. Additionally, impaired movement of the little toe is common, though complete immobility may not always happen. Neglecting these symptoms can worsen the injury and may lead to surgery if the bone does not heal properly. Other signs to watch for with a Jones fracture can include impaired balance, swelling around the fifth metatarsal joint, and bruising around the little toe. Prompt medical attention from a podiatrist, including X-rays for accurate diagnosis and appropriate treatment, is essential for effective healing and preventing long-term complications. If you suspect a Jones fracture or are experiencing any of these symptoms, it is suggested that you schedule an appointment with a podiatrist for proper evaluation and care.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.